ICD-10: How to Avoid These 5
Costly Problems
·
Unspecified Codes Cause a Slowdown
·
Computerized Order Entry
·
Denials Based on Medical Necessity
·
Cash Flow Stops Flowing
·
Clinicians Frustrated, at a Breaking Point
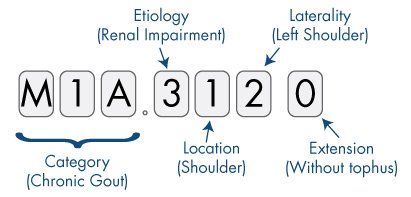
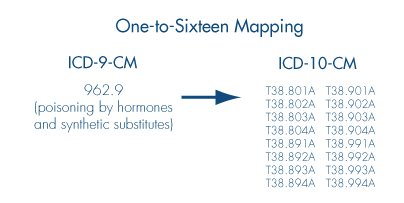
Because ICD-10 is so much bigger than ICD-9, many of the
codes selected by mapping will be unspecified ICD-10 codes. When patients are
seen now, select a specific ICD-10 code. Some of this work could be done by
coders and does not need to be done by the clinician.
Drive out unspecified
ICD-9 codes.
Pay special attention now to the coding denials you're
getting for medical-necessity procedures or treatments. These will only
increase after October 2015. Look at your payer's coverage policies for
procedures and diagnostic tests that you perform or order.
Current payment
methodologies require complete, accurate, and detailed coding in order to
calculate appropriate reimbursement rates, determine coverage, and establish
medical necessity.
Furthermore, with all the quality measures and data
collection, it becomes quite clear that a classification system that provides
greater coding accuracy and specificity was greatly needed. ICD-10 is to provide and meet the goals required with the quality indicators.
Independent of your current E H R System and/or the Practice Management System (PMS), providers will require
all the support to capture, meet and comply with the current
guidelines/regulations to receive payment.
Since 1983 we have been helping physicians to operate practices as a
business, over 500 Medicare and Medicaid audits have given us the knowledge to
develop the AccuChecker Product Line.
ACK has met the previous challenges in the past and is equipped to
meet the new landscape in today’s
healthcare:
·
ICD-10
·
HEDIS
·
PQRS
·
VBM – Valued Base
Modifiers
Call us for more
details.
For more
information on AccuChecker Online or our services:
786-231-7585 or 1-877-938-9311